2022. 10. 20. 10:04ㆍ초음파/유방 검진 & 초음파
Lange Review Ultrasonography Examination, 4th Edition
https://doctorlib.info/ultrasound/review/33.html
Answers and Explanations 10 - Lange Review Ultrasonography Examination, 4th Edition
Lange Review Ultrasonography Examination, 4th Edition Answers and Explanations 1. (B) Breast sonography is an adjunct to mammography in the detection of breast disorders. It is not an examination that is used in place of mammography, but rather in additio
doctorlib.info
https://doctorlib.info/ultrasound/review/34.html
Answers and Explanations 10 - Lange Review Ultrasonography Examination, 4th Edition
Lange Review Ultrasonography Examination, 4th Edition Answers and Explanations 1. (B) Breast sonography is an adjunct to mammography in the detection of breast disorders. It is not an examination that is used in place of mammography, but rather in additio
doctorlib.info
Questions
GENERAL INSTRUCTIONS: For each question, select the best answer. Select only one answer for each question unless otherwise instructed.
1. Which of the following is not an indication for breast ultrasound?
(A) guidance for a breast biopsy
(B) a patient had a breast sonogram last year and prefers it over a mammogram
(C) an abnormality is palpated by the patient’s physician
(D) an abnormality is palpated by the patient
2. Which of the following statements is true regarding focal zone setting in breast sonography?
(A) the focal zone should be set above the level of the lesion being imaged
(B) the focal zone should be set at the level of the lesion being imaged
(C) there should only be one focal zone used for maximum image optimization
(D) the focal zone placement is not critical in sonographic breast imaging
3. What breast lesion is an acoustic standoff pad most helpful?
(A) deep within the breast tissue
(B) axillary in location
(C) superficially positioned within the breast
(D) mobile upon palpation
4. Each breast lesion should be measured in which of the following scan planes?
(A) radial, antiradial
(B) radial, transverse
(C) sagittal, transverse
(D) longitudinal, antiradial
5. A sonographic exam demonstrating a 2 cm anechoic, circumscribed mass at the 4 o’clock position in the left breast is compared to the patient’s mammogram which suggested a 2 cm spiculated mass at the 9 o’clock position. Which of the following should the sonographer do?
(A) tell the patient she has a cyst and there is nothing to worry about
(B) tell the patient that the mammogram was a false positive and she should be followed up with sonography for future evaluation of the mass
(C) take images of all abnormalities and tell the patient she may leave and return next year for her follow-up mammogram
(D) discuss the differences in location and characteristics of the masses seen on the mammogram and sonogram with the interpreting physician.
6. Which of the following best describes the thickness of normal skin overlying the breast?
(A) 2–3 cm
(B) 1–2 cm
(C) 5–10 mm
(D) 2–3 mm
7. While preparing to perform a sonographic exam on a patient who was referred for evaluation of a palpable abnormality, the patient states she cannot feel the area reliably while lying down. Which of the following should the sonographer do?
(A) ask the patient to try and find the lesion lying down because this is the best position for the sonographic exam
(B) ask the patient to find it sitting up because it is usually the easiest position
(C) ask the patient to find the lesion in whatever position necessary and attempt to image it from this position
(D) examine the entire breast without attempting to localize the palpable abnormality
8. Which of the following sonographic features suggests malignancy?
(A) round
(B) posterior acoustic enhancement
(C) spiculated
(D) circumscribed
9. What minimum center frequency in MHz is required for transducers used in breast sonography
(A) 6
(B) 7
(C) 8
(D) 9
(E) 10
10. In order for a breast mass to be characterized as anechoic it must:
(A) not contain any internal echoes
(B) demonstrate reverberation artifacts at the near-field edge
(C) produce refraction artifacts on the lateral borders
(D) demonstrate reduced echogenicity deep to the mass
11. What is the approximate chance of a woman developing invasive breast cancer in her lifetime?
(A) 1 in 8
(B) 1 in 15
(C) 1 in 40
(D) 1 in 100
12. Positioning to reduce the breast thickness of the upper outer quadrant can be achieved by placing the patient in which of the following positions?
(A) place the ipsilateral hand behind the head and roll the patient into an ipsilateral posterior oblique position
(B) place the contralateral hand behind the head and roll the patient into an ipsilateral posterior oblique position
(C) place the ipsilateral hand behind the head and roll the patient into a contralateral posterior oblique position
(D) place the contralateral hand behind the head and roll the patient into a contralateral oblique position
13. Which of the following information is not required documentation for diagnostic sonograms?
(A) laterality (right or left breast)
(B) clock face notation
(C) distance from the nipple
(D) scan plane orientation
(E) patient’s last name only
14. Using the length of the transducer’s footprint may provide a means to determine what sonographic feature of breast abnormalities?
(A) depth of the lesion
(B) distance of the lesion from the nipple
(C) the transverse diameter of the lesion
(D) the depth at which to place the focal zone for best optimization
15. The utilization of the radial/antiradial scan planes provides the best demonstration of what breast anatomy?
(A) the lobes of the glandular tissue
(B) Cooper’s ligaments
(C) the ductal anatomy of the breast
(D) the terminal ductal lobular units
16. Which two characteristics are most helpful to establish concordance between a lesion seen on ultrasound and mammography?
(A) margins and density
(B) echogenicity and distance from the nipple
(C) margins and echogenicity
(D) size and location
17. The mass in Fig. 10–20 can best be described as:
(A) irregular
(B) circumscribed
(C) macrolobulated
(D) spiculated
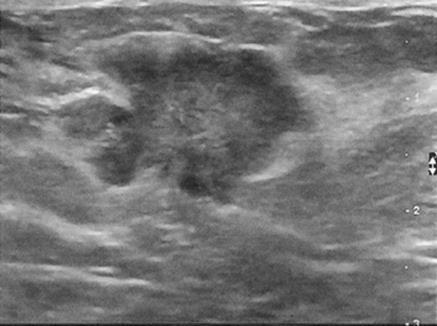
FIGURE 10–20.
18. The mass in Fig. 10–21 is best described as:
(A) round
(B) circumscribed
(C) posteriorly enhancing
(D) spiculated

FIGURE 10–21.
19. In Fig. 10–21, what structure is the arrow pointing to?
(A) Cooper’s ligaments
(B) pectoralis muscle
(C) fibroglandular tissue
(D) skin
20. This image in Fig. 10–22 demonstrates:
(A) dilated ductal anatomy
(B) a simple cyst with breast implant rupture
(C) multiple, irregular cysts
(D) a single cyst with dilated ductal anatomy

FIGURE 10–22.
21. What abnormal finding is not demonstrated in Fig. 10–23?
(A) architectural distortion
(B) posterior acoustic attenuation
(C) angular margins
(D) calcifications

FIGURE 10–23.
22. An asymptomatic patient receives a breast sonogram as additional workup. The exam reveals a mass with multiple internal punctuate echogenic foci. What do these foci most likely represent?
(A) calcifications
(B) gas
(C) artifact
(D) fat
23. Sonography is the recommended initial imaging modality for the evaluation of an area of palpable interest in patients younger than what age?
(A) 30
(B) 40
(C) 50
(D) 60
24. Which of the following terms is not an appropriate descriptor of breast lesion shape?
(A) oblong
(B) round
(C) oval
(D) irregular
25. If sonographic scanning in the upper outer quadrant of the breast demonstrates findings suspicious for a tubular structure, which of the following techniques should be used to further evaluate it?
(A) imaging in an orthogonal plane
(B) use of Doppler
(C) adjusting the gray scale
(D) adjusting the focal zone
26. What type transducer should be used for breast sonography?
(A) curved
(B) linear
(C) vector
(D) curvilinear
27. Echogenicity of a mass is assessed relative to which of the following structures?
(A) Cooper’s ligaments
(B) skin
(C) fat
(D) muscle
28. The appearance of hazy, echogenic material with posterior acoustic shadowing seen in an augmented breast should raise the suspicion for which of the following?
(A) malignancy
(B) scar
(C) fibrocystic disease
(D) implant rupture
29. An image from a sonogram performed on a patient referred for evaluation of a palpable abnormality reveals an oval, circumscribed hypoechoic mass-like area with mixed internal echogenicity seen deep to the pectoralis muscle. What does these findings mostlikely represent?
(A) fibroadenoma
(B) cyst
(C) invasive malignancy
(D) lymph node
(E) rib
30. Which of the following statements is true regarding a biopsy performed with a vacuum-assisted device?
(A) pre-fire and post-fire images should be obtained.
(B) pre-fire images only should be obtained.
(C) post-fire images only should be obtained.
(D) images demonstrating the needle in or adjacent to the mass should be obtained.
31. Which of the following statements is true regarding a breast cyst post-aspiration?
(A) there is no need to acquire a post-aspiration image.
(B) a post-aspiration image should only be obtained if a small amount of fluid remains.
(C) a post-aspiration image should only be obtained if there is question if a solid component is present.
(D) a post-aspiration image should be obtained routinely.
32. During imaging of an area of concern, there is evidence of interruption of the Cooper’s ligaments. An irregular hypoechoic region with angular margins and posterior acoustic shadowing is seen, but no mass is visualized. Which of the following is the most appropriate descriptor for this appearance?
(A) spiculation
(B) architectural distortion
(C) dirty shadowing
(D) normal parenchyma
33. The finding discussed in question 32 is most likely to be seen in which of the following scenarios?
(A) benign lesions
(B) post-surgical change
(C) young, asymptomatic patients
(D) pregnant patients with a palpable mass
Lange Review Ultrasonography Examination, 4th Edition
Answers and Explanations
1. (B) Breast sonography is an adjunct to mammography in the detection of breast disorders. It is not an examination that is used in place of mammography, but rather in addition and is not used alone as a screening tool. A, C and D are all indications for breast sonography. (Study Guide)
2. (B) Placement of the focal zone at the level of the lesion or region of interest optimizes visualization of the lesion characteristics. (Study Guide)
3. (C) The use of an standoff pad improves visualization of superficial lesions within the near field, which is sometimes referred to as the sonographic ‘blind spot’. (Study Guide)
4. (A) Radial and antiradial are the preferred scan planes for imaging the breast anatomy primarily based on the ductal anatomy of the breast as it converges toward the nipple. The annotation of the clock face orientation for imaging denotes transducer placement for radial/antiradial scan planes. (Study Guide)
5. (D) All sonographic findings should be discussed with the interpreting physician. (Study Guide)
6. (D) Skin thickness is normally no more than 2–3 mm. (Study Guide)
7. (C) Localizing a palpable lesion is paramount to the performance of an adequate exam. It is also important to stabilize the lesion so that it may be adequately examined. This is often best achieved by scanning the patient in the position in which the lesion is best felt. (Study Guide)
8. (C) Spiculated borders of a breast mass are considered abnormal and concerning for malignancy. (Study Guide)
9. (B) A minimum center frequency of 7 MHz is required for breast sonography, although higher frequencies should be employed when possible. Superficial lesions or smaller breast mass would not require as much penetration and a higher frequency would be appropriate. (Study Guide)
10. (A) The term anechoic indicates ‘without echoes’ and therefore, for a lesion to be deemed such, it should not produce any echoes within. Cysts may produce reverberation artifacts in the near-field edge, but this is not a requirement to be deemed anechoic. (Study Guide)
11. (A) The chance of developing breast cancer in a woman’s life is approximately 1 in 8. (Study Guide)
12. (C) This position permits placement of the breast tissue on a level surface and reduces breast thickness in the upper outer quadrant. (Study Guide)
13. (E) All images are considered part of a patient’s medical record and should document the patient’s full name. (Study Guide)
14. (B) The distance of a lesion from the nipple should be documented with as much accuracy as possible. By knowing the length of the transducer’s footprint that distance can be assessed by placing the edge of the transducer at the nipple and evaluating the relationship of the lesion’s position to the transducer edge in terms of a ratio of the transducer length. (Study Guide)
15. (C) The ductal anatomy of the breast converges toward the nipple. The implementation of the radial and antiradial scan planes provides longitudinal and transverse orientation with respect to breast anatomy. (Study Guide)
16. (D) In order to compare sonographic findings with mammography, it is important to verify that location and the lesion size are consistent in order to prevent errors of discordance. (Study Guide)
17. (A) The lesion is not circumscribed. Macrolobulation is typically benign descriptor that is best reserved for an oval benign-appearing mass such as a suspected fibroadenoma. A spiculated appearance is typically seen with more hypoechoic masses, posterior acoustic shadowing and architectural distortion, similar to that seen with postsurgical scarring. (Study Guide)
18. (B) The lesion is oval and circumscribed, typical for a fibroadenoma. (Study Guide)
19. (B) The pectoralis muscle is demonstrated posterior to the breast tissue and is recognized by internal echogenic striations. (Study Guide)
20. (D) This image demonstrates a well-circumscribed anechoic lesion with posterior enhancement suggesting a breast cyst. In close proximity to the cyst, there are tubular hypoechoic structures suggesting dilated ducts are present. (Study Guide)
21. (D) There are no calcifications suggested in this image, although there is distortion of the normal breast tissue with angular margins and some posterior acoustic shadowing/attenuation. (Study Guide)
22. (A) Artifactual internal echogenicity and fat are rarely punctuate in appearance. Additionally, gas would be unlikely in an asymptomatic patient. (Study Guide)
23. (A) Younger patients typically have dense glandular breast tissue, which prevents mammography from clearly identifying abnormalities even if palpable. The use of sonography can not only evaluate the area of interest, but also correlate any findings with palpation while reducing the patient’s exposure to ionizing radiation. (Study Guide)
24. (A) Oblong is not an accepted descriptor of lesion shape. (Study Guide)
25. (B) Imaging in the orthogonal plane is necessary for any evaluation in breast sonography, normal or abnormal. The use of Doppler will help determine if this finding is a vessel or a duct. (Study Guide)
26. (B) Linear array transducers provide the best resolution and are particularly useful in superficial structures, such as the breast, when a wide field of view is not essential. (Study Guide)
27. (C) Fat is hypoechoic relative to the mammary/glandular tissue. The gray scale and gain settings should be set to demonstrate fat as the medium level echo and compare all other tissue/findings to its echogenicity (Study Guide)
28. (D) Free silicone has the appearance of ‘dirty shadowing’, which is described in this question. (Study Guide)
29. (E) The ribs and chest wall are the only structures which are typically identified deep to the pectoralis muscle. Lymph nodes in this region are not commonly identified by ultrasound. (Study Guide)
30. (D) Vacuum-assisted devices do not ‘fire’ when obtaining the specimen. (Study Guide)
31. (D) This protocol is important to determine and document the completeness of the aspiration. (Study Guide)
32. (B) Spiculation is used to describe the margins of a mass when the tissue surrounding the mass is altered and has angular characteristics. Architectural distortion is best used when a mass is not appreciated, but the tissue is similarly altered. (Study Guide)
33. (B) Architectural distortion is usually seen post-surgically or in association with a malignancy. (Study Guide)
'초음파 > 유방 검진 & 초음파' 카테고리의 다른 글
| 유방초음파_이론 (0) | 2022.10.20 |
|---|